Transdermal patches have become a popular method of drug delivery, offering a convenient and non-invasive way to administer medications. These patches deliver drugs through the skin and directly into the bloodstream, providing controlled and sustained release. There are several types of transdermal patches, each designed for specific drugs and therapeutic purposes. In this detailed guide, we’ll explore the various types of transdermal patches and their unique characteristics.
What is a Transdermal Patch?
A transdermal patch is a method of drug delivery in which a patch containing medication is applied to the skin. The medication is absorbed through the skin and enters the bloodstream, providing a steady and controlled release of the drug over time. This non-invasive approach offers an alternative to oral or injectable medications, allowing for consistent drug levels and reduced side effects.
Transdermal patches are commonly used for pain relief, nicotine replacement therapy, hormone therapy, and motion sickness prevention. The patch consists of a backing layer, drug layer or reservoir, adhesive, and a protective liner. It’s applied to clean, dry skin and replaced according to the prescribed schedule.
Transdermal patches are favoured for their convenience, ease of use, and ability to bypass the digestive system, ensuring more direct delivery of the medication to the bloodstream. In 2023, the global transdermal patches market was estimated to be worth $6.2 billion. It is projected to reach $8.0 billion by 2029, exhibiting a compound annual growth rate (CAGR) of 4.5%.
How to Make a Transdermal Patch
Creating a transdermal patch involves several steps and components to ensure effective drug delivery through the skin:
- Design the Patch: Determine the size, shape, and type of patch based on the drug’s properties and the desired release rate. Select the appropriate materials for each layer of the patch.
- Prepare the Drug Layer: Mix the active pharmaceutical ingredient (API) with excipients, such as penetration enhancers, stabilizers, and solvents, to create a homogenous drug formulation. This can be done in the form of a reservoir or a matrix within the patch.
Construct the Patch Layers:
- Backing Layer: Choose a material that is impermeable to the drug and excipients, providing protection and structural support.
- Drug Layer/Reservoir: Apply the drug formulation onto the backing layer or encapsulate it in a separate reservoir.
- Adhesive Layer: Select a biocompatible adhesive that can hold the patch on the skin and, if necessary, aid in drug delivery.
- Release Liner: Apply a release liner to protect the adhesive layer before application, which is removed before use.
Laminate the Layers: Carefully laminate the layers together, ensuring airtight seals to prevent leakage or contamination.
Cut and Package: Use precision cutting tools to cut the laminated sheets into individual patches. Package each patch in a protective pouch to maintain sterility and shelf life.
Quality Control: Conduct thorough testing to ensure the patch meets safety, efficacy, and quality standards, including drug release rate, adhesion properties, and shelf life.
Remember, each transdermal medication patch may vary based on the drug being administered, but the basic elements remain consistent: backing layer, active drug, and release liner.
Types of Transdermal Patches
Transdermal patches have revolutionized the way medications are administered, offering a convenient and non-invasive alternative to traditional oral or injectable routes. These patches deliver drugs directly through the skin and into the bloodstream, providing controlled and sustained release over an extended period. The versatility of transdermal patches has led to the development of various types, each designed to cater to specific medical requirements and drug delivery needs:
Single-Layer Drug-in-Adhesive Patches:
In these patches, the drug is incorporated directly into the adhesive layer that sticks to the skin. This design simplifies the patch structure and manufacturing process, making it cost-effective for mass production. The single-layer approach is suitable for drugs that are compatible with adhesive materials and require a steady release rate.
Multi-Layer Drug-in-Adhesive Patches:
These patches feature multiple layers of drug-in-adhesive, allowing for more complex drug release profiles. They can be used to deliver different drugs sequentially or to provide an initial burst of medication followed by a sustained release. Multi-layer patches are beneficial for treatments that require a combination of fast-acting and long-lasting effects.
Reservoir Patches:
Reservoir patches contain a separate compartment for the drug, typically in liquid or gel form, controlled by a rate-limiting membrane. The membrane’s properties determine the rate at which the drug is released, offering precise control over dosage. These patches are often used for potent drugs that require strict control over blood concentration levels.
Matrix Patches:
In matrix patches, the drug is dispersed within a polymer matrix that directly contacts the skin. As the matrix interacts with skin moisture, the drug is released at a controlled rate. This design is suitable for drugs that are stable within a polymer matrix and do not require a separate reservoir.
Vapour Patches:
Vapor patches release volatile substances in the form of vapor, which can be absorbed through inhalation or the skin. They are commonly used for respiratory therapies, such as nasal decongestants, or for aromatherapy applications. The simplicity of vapor patches makes them ideal for over-the-counter products.
Micro-needle Patches:
These patches contain tiny needles that create microchannels in the skin, enhancing permeability for drug delivery. Micro-needle patches can deliver larger molecules, such as proteins and vaccines, that cannot passively diffuse through the skin. They offer a painless alternative to traditional injections and are being explored for various therapeutic applications.
Iontophoretic Patches:
Iontophoretic patches use electrical currents to drive charged drug molecules through the skin, enhancing absorption. This active delivery method is suitable for drugs that are difficult to deliver through passive diffusion. Applications include local anesthesia, anti-inflammatory treatments, and drug delivery for specific skin conditions.
Ultrasound Patches:
Ultrasound patches employ ultrasound waves to temporarily increase skin permeability, allowing for enhanced drug delivery. They are being investigated for the delivery of large molecules and targeted drug delivery to specific tissues or organs. This technology has the potential to expand the range of drugs that can be delivered transdermally.
Heat-Activated Patches:
Heat-activated patches use a temperature-sensitive mechanism to control the release of the drug. The application of heat, either externally or through body temperature, triggers the release of the medication. These patches are useful for conditions that benefit from localized heat, such as muscle pain or menstrual cramps.
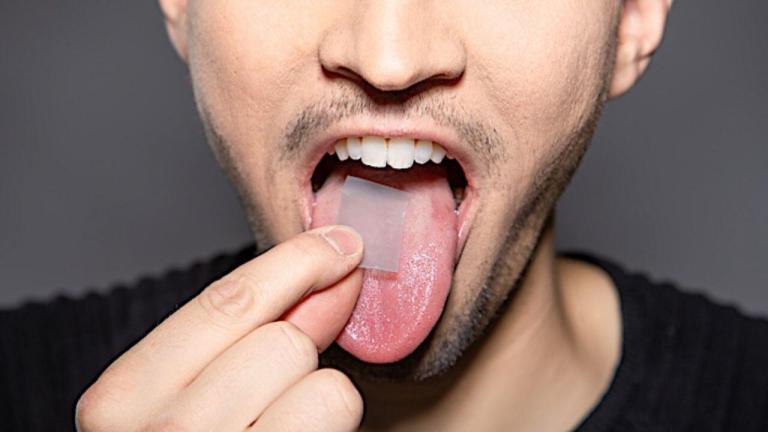
Bioadhesive Patches:
Bioadhesive patches utilize biocompatible adhesive materials that interact with biological tissues to enhance adhesion and drug absorption. They are particularly useful for mucosal delivery, where traditional adhesives may not be effective. Applications include buccal, ocular, and vaginal drug delivery systems.
Hydrogel Patches:
Hydrogel patches consist of a water-based gel matrix that provides a moist environment for drug delivery. They are commonly used for wound care, delivering antimicrobial agents or pain relievers directly to the affected area. The hydrogel matrix is gentle on the skin and can be formulated to release drugs at a controlled rate.
Pressure-Sensitive Patches:
Pressure-sensitive patches release medication in response to applied pressure, allowing for on-demand drug delivery. These patches are useful for conditions that require intermittent dosing or for patients who need control over their medication timing.
The technology is being explored for applications in pain management and other therapeutic areas.
Transdermal patches are generally safe, but accidental exposure can occur. Over a 10-year period, there were 6,746 adult exposures and 1,917 pediatric exposures to transdermal drug delivery systems (TDDS). Here’s a table summarizing the differences between the various types of transdermal patches:
| Type of Patch | Description | Advantages | Applications |
| Single-Layer Drug-in-Adhesive | Drug is incorporated into the adhesive layer. | Simple design, cost-effective, steady release rate. | Nicotine patches, hormone replacement therapy. |
| Multi-Layer Drug-in-Adhesive | Multiple layers of drug-in-adhesive for complex release profiles. | Allows sequential or simultaneous release of multiple drugs. | Treatments requiring fast-acting and long-lasting effects. |
| Reservoir | Separate compartment for the drug, controlled by a rate-limiting membrane. | Precise control over dosage, suitable for potent drugs. | Pain relievers, hormonal therapies. |
| Matrix | Drug dispersed within a polymer matrix in direct contact with the skin. | Suitable for drugs stable in a polymer matrix, steady release rate. | Various medications requiring steady release. |
| Vapor | Releases volatile substances in vapor form, absorbed through inhalation or skin. | Simple design, ideal for over-the-counter products. | Nasal decongestants, aromatherapy. |
| Micro-needle | Contains tiny needles that create microchannels in the skin. | Painless alternative to injections, can deliver larger molecules. | Vaccines, protein-based drugs. |
| Iontophoretic | Uses electrical currents to drive charged drug molecules through the skin. | Enhances absorption of difficult-to-deliver drugs. | Local anesthesia, anti-inflammatory treatments. |
| Ultrasound | Employs ultrasound waves to increase skin permeability. | Potential for delivery of large molecules and targeted drug delivery. | Research and development stage. |
| Heat-Activated | Uses temperature-sensitive mechanism to control drug release. | Useful for conditions benefiting from localized heat. | Muscle pain, menstrual cramps. |
| Bioadhesive | Utilizes biocompatible adhesive materials for enhanced adhesion and drug absorption. | Effective for mucosal delivery, gentle on biological tissues. | Buccal, ocular, vaginal drug delivery systems. |
| Hydrogel | Water-based gel matrix providing a moist environment for drug delivery. | Gentle on the skin, suitable for wound care and controlled release. | Wound care, antimicrobial agents, pain relievers. |
| Pressure-Sensitive | Releases medication in response to applied pressure. | Allows for on-demand drug delivery, control over medication timing. | Pain management, intermittent dosing needs. |
Each type of transdermal patch has distinct characteristics and is chosen based on the specific requirements of the medication and the patient’s needs.
What are the Benefits of Transdermal Patches Over Others?
Transdermal patches offer a range of benefits as a drug delivery system, making them a popular choice for both patients and healthcare providers. Here are some of the key advantages:
- Controlled Release: Transdermal patches provide a steady, controlled release of medication over an extended period, ensuring consistent drug levels in the bloodstream. This can enhance the therapeutic efficacy of the drug and reduce the frequency of dosing, improving patient compliance.
- Non-Invasive: Unlike injections or intravenous therapy, transdermal patches are non-invasive and painless. This makes them particularly suitable for patients who have a fear of needles or for long-term treatments that require frequent dosing.
- Bypassing the Gastrointestinal Tract: Transdermal patches deliver medication directly into the bloodstream through the skin, bypassing the gastrointestinal tract. This avoids the first-pass metabolism in the liver, which can reduce the drug’s effectiveness, and minimizes gastrointestinal side effects such as nausea and vomiting.
- Easy to Use: Patches are simple to apply and can be self-administered by patients. They are discreet and can be worn under clothing, allowing for normal daily activities without interference.
- Reduced Systemic Side Effects: Because transdermal patches deliver medication directly to the site of action or into the systemic circulation, they can reduce the risk of systemic side effects compared to oral medications that affect the entire body.
- Targeted Delivery: Some transdermal patches are designed to deliver medication to a specific area of the body, providing targeted relief for localized conditions such as pain or inflammation.
- Versatility: Transdermal patches can be formulated to deliver a wide range of medications, including hormones, pain relievers, nicotine, and more. They can be tailored to suit different dosing requirements and patient preferences.
- Removal at Any Time: If adverse reactions occur or if the medication is no longer needed, the patch can be easily removed, quickly stopping the drug’s delivery.
- Improved Adherence: The convenience and ease of use of transdermal patches can lead to improved adherence to treatment regimens, especially for chronic conditions that require long-term medication.
- Less Frequent Dosing: Because transdermal patches provide a sustained release of medication, they often require less frequent dosing than oral medications, which can improve patient convenience and compliance.
Drugs That are Administered Through Transdermal Patches
Transdermal patches are used to administer a variety of drugs for different medical conditions. Transdermal patches are a highly effective method for delivering drugs through the skin. These patches have the remarkable ability to retain up to 95% of the initial total amount of drug even after the intended wearing period.
For instance, oestradiol patches, frequently utilized in hormone replacement therapy, demonstrate significant drug retention rates.
Here are some types of drugs commonly delivered through transdermal patches:
- Nicotine: Used for smoking cessation, nicotine patches help reduce withdrawal symptoms and the urge to smoke by delivering a controlled amount of nicotine through the skin.
- Hormones: Hormonal patches are used in hormone replacement therapy, delivering hormones like estrogen and testosterone to treat symptoms of menopause or hormonal imbalances. Contraceptive patches, which release a combination of estrogen and progestin, are used for birth control.
- Pain Relievers: Opioid analgesics like fentanyl and buprenorphine are available in patch form for managing chronic pain, offering sustained relief without the need for frequent dosing.
- Antihypertensives: Some patches contain antihypertensive medications to help control high blood pressure by delivering the drug steadily over time.
- Neurological Medications: Patches containing drugs like rivastigmine and rotigotine are used to treat neurological disorders such as Alzheimer’s disease and Parkinson’s disease, respectively, by providing a continuous supply of medication.
- Anti-anginal Drugs: Nitroglycerin patches are used to prevent angina (chest pain) in people with heart disease by delivering the drug directly into the bloodstream.
- Motion Sickness Medication: Scopolamine patches are used to prevent nausea and vomiting associated with motion sickness by delivering the drug transdermally.
- Vitamin and Mineral Supplements: Some patches are designed to deliver vitamins and minerals, such as vitamin B12 or vitamin D, to individuals who may have deficiencies or absorption issues.
Development and Manufacturing of Transdermal Patches
The Drug Development Process
The development and manufacturing of transdermal patches in the United States adhere to strict guidelines set by the Food and Drug Administration (FDA). The process involves several key stages:
- Discovery and Development: This initial phase involves laboratory research to develop new chemical compounds, gain insights into existing diseases, and devise new drug processing technologies.
- Preclinical Research: The safety of the drug is evaluated through laboratory and animal testing to address fundamental safety questions.
- Clinical Research: The drug undergoes testing on human subjects to confirm its safety and efficacy.
- FDA Review: The FDA thoroughly reviews all submitted data to determine whether the drug or device meets the required standards for approval.
- Post-Market Safety Monitoring: Once the product is available to the public, the FDA continues to monitor its safety.
Manufacturing Process for Transdermal Patches
Developing a new drug and producing a transdermal patch can be complex and challenging. The manufacturing process typically involves three main steps:
- Mixing: The adhesive is mixed with the active drug and any necessary excipients to create a homogeneous and stable mixture. This step requires careful consideration of the materials, properties of the desired product, and the appropriate equipment.
- Coating: The mixture is then precisely applied to a polymer liner and sealed in a convection oven. This stage demands a deep understanding of temperature control, the chemical behavior of the drug, and precise oven placement to ensure the drug’s integrity.
- Converting and Packaging: The final stage involves converting the laminate into individual patches and packaging each one in a pouch. While this step may seem straightforward, it is crucial for preserving the delivery system’s integrity. Any errors during this stage can result in the loss of a significant number of patches.
Throughout the manufacturing process, it is essential to have trained engineers and specialized equipment to ensure the production of high-quality transdermal patches that meet regulatory standards and effectively deliver medication to patients.
Final Words
Each type of transdermal patch has its unique advantages and applications, tailored to the specific properties of the medication and the therapeutic needs of the patient. The choice of patch type depends on factors such as the drug’s molecular size, required release rate, and the desired duration of treatment. Transdermal patches offer a promising avenue for drug delivery, combining convenience, safety, and efficacy to enhance patient care and treatment outcomes.