Overview
Efficient Transition Between Phases: The transition between different phases of clinical trials is a complex process that requires meticulous planning and execution. Our approach ensures a smooth transition from early preclinical discovery through to late-stage clinical development. We employ a proactive strategy that anticipates phase-specific requirements, thereby minimizing the risk of delays. This involves close coordination with cross-functional teams to align on timelines, resource allocation, and regulatory milestones, ensuring that each phase progresses without interruption.
Data Continuity and Integrity: The integrity of clinical trial supply data is paramount. Our rigorous data management practices involve the implementation of robust information systems that ensure data continuity and enhance its integrity across all trial phases. This comprehensive data management strategy provides a complete understanding of the investigational drug’s safety and efficacy profile, which is crucial for the success of clinical trial supply chains. We employ advanced data analytics tools to monitor and analyze supply chain data, ensuring that decision-making is informed by accurate, real-time information.
Resource Optimization: Resource optimization is a key objective in our clinical trial supply process. We strive to use all resources efficiently, ensuring that planning and allocation are optimized to prevent waste and streamline operations across every phase of the clinical trial supply process. This includes the strategic use of inventory, minimizing overstock and understock situations, and leveraging just-in-time delivery methods to reduce storage costs and maximize the use of available space.
Regulatory Strategy: Our regulatory strategy is designed to evolve alongside the drug development process. We foster improved communication with regulatory bodies through a unified approach that addresses the complex and ever-changing regulatory landscape. This involves staying abreast of new regulations, guidelines, and best practices, as well as engaging with regulatory agencies early and often to ensure compliance and expedite approvals.
Adaptive Trial Design: Our clinical trial services support adaptive trial designs, which allow for real-time protocol adjustments based on interim results. This flexibility enhances the probability of trial success and ensures a more responsive clinical trial supply framework. Adaptive trial designs require a dynamic supply chain capable of adjusting to changes in trial parameters, such as patient enrollment rates, dosing schedules, and site locations.
Cost Management: Cost management is a critical aspect of clinical trial supply. Our services are designed to reduce the need for repeated setups for each phase, enabling precise budget forecasting and financial planning. This approach ensures economic efficiency by minimizing unnecessary expenditures and optimizing the use of financial resources throughout the trial.
Quality Assurance: Quality assurance is integral to our clinical trial supply services. We implement a comprehensive quality management system that encompasses all aspects of the supply chain, from procurement to distribution. This results in a robust and reliable data set for regulatory submission, reflecting the high standards of our clinical trial supply services.
Market Readiness: Reducing downtime between clinical phases is a key goal for efficient clinical trial supply. We focus on accelerating the drug’s journey to market, ensuring that your company is poised to meet market needs swiftly. This involves strategic planning to align clinical trial timelines with market launch objectives, ensuring that investigational drugs are ready for commercialization as soon as regulatory approvals are obtained.
Clinical Trial Supply Chain Management
Inventory Management: Effective inventory management is crucial to ensure that all necessary materials are available when needed without excess. We employ sophisticated inventory management systems that provide real-time visibility into stock levels, enabling proactive replenishment and reducing the risk of stockouts or overstock.
Distribution Logistics: Our clinical trial supply chain is designed for efficient distribution, ensuring the timely delivery of clinical trial materials to global sites. We leverage a network of distribution centers and advanced logistics solutions to manage the complexities of global shipping, customs clearance, and last-mile delivery.
Clinical Trial Supply Forecasting
Demand Planning: Accurate demand planning is a key aspect of clinical trial supply, allowing for the anticipation of material requirements and avoiding shortages or overstock. We utilize forecasting models that incorporate historical data, enrollment projections, and site-specific considerations to predict material needs accurately.
Supply Chain Analytics: We use advanced analytics in our clinical trial supply chain to predict and respond to potential challenges proactively. This includes the use of predictive modeling, simulation, and scenario analysis to identify risks and opportunities within the supply chain.
Stakeholder Engagement: Active engagement with stakeholders is a critical component of clinical trial supply. We maintain open lines of communication with all parties involved, from suppliers to healthcare professionals, to ensure that the clinical trial supply chain operates smoothly and efficiently.
Environmental Sustainability: Environmental sustainability is becoming increasingly important in clinical trial supply. We strive to implement eco-friendly practices in our supply chain, reducing the environmental impact while maintaining the highest standards of clinical trial supply. This includes the use of sustainable packaging materials, optimization of transportation routes to reduce carbon emissions, and the implementation of recycling programs.
Phase-Specific Solutions
Phase I – Early Development
Formulation Development: In the initial phase of drug development, the formulation team focuses on creating formulations suitable for first-in-human (FIH) trials. This involves a meticulous process of selecting excipients that are safe and compatible with the active pharmaceutical ingredient (API), while also considering the intended route of administration. The goal is to ensure safety, stability, and scalability. The formulations are designed to be robust enough to maintain their integrity under various conditions and scalable for future production increases.
Analytical Development: Analytical methods are developed and validated to ensure that the clinical trial materials (CTMs) meet the highest quality standards. These methods are used to test the identity, purity, potency, and stability of the API and the final formulated product. Advanced analytical techniques such as high-performance liquid chromatography (HPLC), mass spectrometry (MS), and nuclear magnetic resonance (NMR) spectroscopy are commonly employed.S
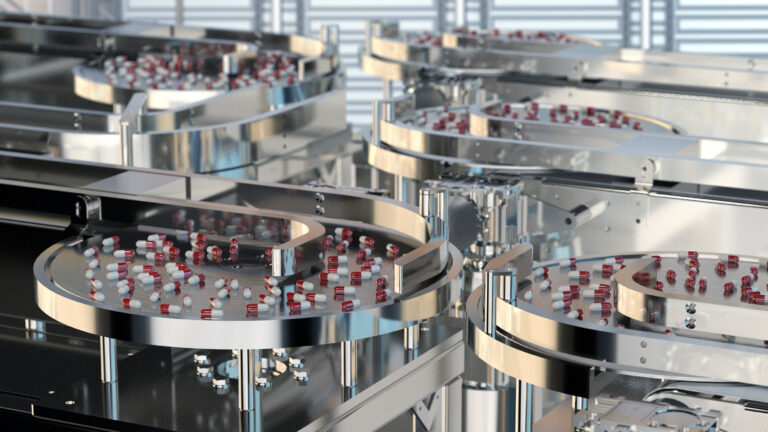
Precision Manufacturing: Clinical batches are produced with precision to meet the stringent requirements of initial dosing studies. This involves the use of Good Manufacturing Practice (GMP) facilities and processes to ensure that each batch is consistent and reproducible. The manufacturing process is closely monitored to ensure that the product meets predefined specifications.
Strategic Regulatory Insight: Regulatory strategy is integral to the early stages of clinical development. Expert teams provide guidance on Investigational New Drug (IND) filings and help navigate the complex regulatory landscape. This proactive approach aims to streamline the process, reduce the risk of regulatory setbacks, and expedite the timeline for clinical trials.
Phase II – Proof Of Concept
Optimized Dosing: Dosing strategies are refined based on data obtained from Phase I trials. The objective is to find the optimal balance between efficacy and safety, which may involve adjusting the dose strength or frequency. This phase often includes dose-ranging studies to determine the most effective dose with the least side effects.
Process Scale-Up: Transitioning from lab-scale to pilot-scale production is a critical step in Phase II. This scale-up process must be carefully managed to maintain the quality and efficiency of the product. It involves scaling up the manufacturing process, validating the process at the pilot scale, and ensuring that the product remains stable and consistent.
Stability Protocols: Stability studies are an essential part of Phase II, providing data on how the quality of a drug substance or drug product varies with time under the influence of environmental factors such as temperature, humidity, and light. These studies help to establish shelf life and recommended storage conditions.
Patient-Centered Formulation: Formulations are designed with the patient’s needs in mind, aiming to enhance the treatment experience and adherence. This may involve developing patient-friendly dosage forms, such as orally disintegrating tablets or transdermal patches, and considering factors like taste masking and ease of administration.
Phase III – Final Studies
Scalable Manufacturing: In Phase III, manufacturing capabilities are expanded to accommodate large-scale production, which is necessary to meet the demands of extensive clinical trials involving large patient populations. This requires a significant investment in manufacturing infrastructure and technology to ensure that production can be scaled up without compromising product quality.
Global Regulatory Mastery: Regulatory expertise becomes even more critical as the clinical trial expands to multiple regions. Teams must navigate the regulatory requirements of different countries, manage multi-regional clinical trial applications, and ensure global compliance.
Efficient Supply Chain: The logistics of the clinical trial supply chain are optimized for efficiency and reliability. This includes managing the distribution of CTMs to global trial sites and ensuring that sites have an adequate supply of the product when needed.
Market Readiness: Preparations for market launch begin in Phase III. This involves laying the groundwork for commercialization, including planning for manufacturing scale-up, marketing, and post-marketing surveillance.
Phase IV – Post-Marketing
Post-Launch Monitoring: After a drug is launched, ongoing monitoring is conducted to track its safety and efficacy in the general population. This phase involves pharmacovigilance activities, including the collection and analysis of adverse event data.
Lifecycle Management: The focus on cost reduction and process improvement continues even after the drug has been launched. This includes optimizing manufacturing processes and exploring new indications for the drug to enhance its value.
Support for Additional Indications: Post-marketing studies may be conducted to support the approval of additional indications for the drug. This involves conducting supplemental studies and submitting the data to regulatory authorities for label expansion.
Quality Management: Maintaining consistent product quality is crucial throughout the drug’s lifecycle. Quality management systems are in place to ensure that the product continues to meet all quality standards and regulatory requirements.
Formulation Development
Advanced Bioavailability Techniques: Bioavailability is a critical parameter in drug development, influencing both the efficacy and safety of pharmaceutical agents. Advanced techniques aim to overcome the common challenges of poor solubility and permeability, which can hinder a drug’s therapeutic potential.
Nanoparticle Technology: Nanoparticles, with their sub-micron size, offer a vast surface area relative to their volume, enhancing the dissolution and absorption rates of drugs. These tiny carriers can be engineered to encapsulate drugs, protecting them from degradation and targeting them to specific sites within the body. The use of polymeric nanoparticles, liposomes, and solid lipid nanoparticles are examples of how this technology can be tailored to improve bioavailability.
Lipid-Based Formulation: Lipid-based formulations, such as self-emulsifying drug delivery systems (SEDDS), utilize the body’s natural lipid digestion and absorption pathways. By incorporating drugs into lipid vehicles, they can be solubilized and absorbed more efficiently, particularly for drugs with poor water solubility.
Solubility Enhancement: Techniques like salt formation, co-solvents, and pH adjustments are employed to enhance the solubility of APIs. Complexation with cyclodextrins, for instance, can improve the solubility and stability of hydrophobic drugs, making them more bioavailable.
Permeability Optimization: Strategies to enhance permeability include the use of permeation enhancers, which temporarily disrupt the cell membrane to allow drug passage, and efflux inhibitors, which prevent the active efflux of drugs from cells, thereby increasing their intracellular concentrations.
Formulation Development and Optimization
Co-Crystallization: This technique involves forming a crystalline complex between the API and a co-former, which can improve the drug’s physicochemical properties, such as solubility and stability, without altering its pharmacological activity.
Hot-Melt Extrusion: Hot-melt extrusion is used to produce amorphous solid dispersions, which can significantly enhance the dissolution rate and bioavailability of poorly soluble drugs. The process involves the melting of the drug with a polymer and then shaping the molten mix into a solid dispersion as it cools.
Customized Drug Delivery Systems
Targeted Delivery Design: Targeted drug delivery systems, such as microspheres and microcapsules, can be designed to release drugs at specific sites, reducing systemic side effects and improving therapeutic efficacy.
Osmotic Pump Tablets: These tablets use osmotic pressure to deliver drugs at a controlled rate over an extended period, offering the advantage of maintaining consistent plasma drug levels.
Formulation Development Technologies
Advanced Delivery Systems: Technologies like multiparticulate systems enable the modulation of drug release profiles, allowing for delayed, sustained, or pulsatile drug release, which can be crucial for drugs with narrow therapeutic windows or those requiring chronotherapy.
Excipient Synergy: The selection of excipients is a strategic process, where excipients are chosen not only for their compatibility and stability-enhancing properties but also for their ability to interact synergistically with the drug to improve its release and absorption.
Process Development
Scalable Techniques: Scalable manufacturing techniques are essential for the transition from small-scale laboratory production to large-scale commercial manufacturing, ensuring that quality is maintained at every scale.
Process Analytical Technology (PAT): PAT tools are employed for real-time monitoring and control of the manufacturing process, ensuring consistent product quality and enabling a more efficient and responsive production environment.
Regulatory Considerations in Pharmaceutical Development
Regulatory considerations are integral to pharmaceutical development, ensuring that products are safe, effective, and of high quality. Regulatory agencies, such as the FDA and EMA, provide guidelines and requirements that pharmaceutical companies must adhere to throughout the drug development process.
Chemistry, Manufacturing, and Controls (CMC): CMC considerations encompass the entire process of drug development, from the synthesis of the drug substance to the final drug product’s manufacturing. This includes ensuring the quality of raw materials, the stability of the drug substance, and the reproducibility of the drug product’s manufacturing process.
Good Manufacturing Practice (GMP): GMP standards are followed to ensure that products are consistently produced and controlled according to quality standards. This covers all aspects of production, from the starting materials to the training of personnel.
Regulatory Submissions: Detailed documentation is required for regulatory submissions, including the Investigational New Drug (IND) application, New Drug Application (NDA), and Biologics License Application (BLA). These documents must provide comprehensive information on the drug’s formulation, manufacturing process, quality control, and preclinical and clinical data.
Post-Approval Changes: After a drug is approved, any changes to the manufacturing process, formulation, or packaging must be submitted for regulatory review. This ensures that the changes do not impact the product’s safety, efficacy, or quality.
Manufacturing Capabilities
Facility and Equipment Excellence:
GMP-Certified Facilities: Our facilities are not just buildings where products are made; they are the very foundation of our promise to deliver quality. Each facility is GMP-certified, which means they adhere to the Good Manufacturing Practice regulations enforced by the FDA. These regulations are not static; they evolve to incorporate the latest in scientific and processing advancements, ensuring that the facilities are not just meeting but exceeding the rigorous standards set forth for drug manufacturing. This commitment to quality is not just about compliance; it’s about going above and beyond to ensure that every product that comes out of our facilities can be trusted for its quality, safety, and efficacy.
State-of-the-Art Equipment: In the pharmaceutical industry, the equipment used can be as important as the facility itself. We invest in the most advanced manufacturing equipment available, which is a vital component of our clinical trial supply chain. This equipment is selected and maintained to ensure optimal production efficiency, which translates to reliability and speed in drug development and delivery. The state-of-the-art equipment allows us to maintain a competitive edge, ensuring that we can produce complex formulations and meet the precise needs of modern medicine.
Automated Systems: Automation is key to precision in pharmaceutical manufacturing. Our automated systems ensure exact dosing and packaging, which are crucial for clinical trial supply. These systems are designed to guarantee consistency and compliance with the stringent requirements of clinical trials. Automation reduces the potential for human error, increases efficiency, and ensures that every product is consistent with the last, providing reliability that clinicians and patients can depend on.
Scalability and Flexibility:
Agile Processes: The pharmaceutical market is dynamic, with demands that can change rapidly. Our agile manufacturing processes are essential for clinical trial supply scalability. They are designed for rapid scale-up, allowing us to meet the growing and often unpredictable demands of the market. This agility ensures that we can respond quickly to new opportunities or urgent needs, such as those that arise during public health emergencies.
Versatile Production Lines: Versatility in production lines is a strategic advantage. It supports the clinical trial supply chain by allowing quick transitions between products. This reduces downtime and maximizes output, ensuring that we can pivot as needed without significant delays. It’s a testament to our commitment to being responsive and adaptable in a fast-paced industry.
Quality and Compliance:
Integrated Quality Control: Quality control is not a checkpoint; it’s an integrated system that spans the entire manufacturing process. Our integrated quality control systems are a cornerstone of clinical trial supply, providing continuous monitoring to ensure that every product meets stringent standards. This system is part of a larger quality management strategy that encompasses every step from raw material selection to final product release.
Global Regulatory Adherence: In a global market, compliance with international regulatory requirements is not just essential; it’s a complex challenge that we navigate daily. Our adherence to global regulatory standards ensures that our products can be accessed by markets worldwide. This global perspective is critical for a supply chain that must be as diverse and far-reaching as the patients it serves.
Innovation in Manufacturing:
Continuous Technological Investment: Innovation is driven by continuous technological investment. Our commitment to this principle drives innovation in clinical trial supply, enhancing both drug formulation and production. By investing in new technologies, we can explore novel drug delivery systems, improve manufacturing processes, and ultimately bring better products to market faster.
Sustainable Manufacturing: Sustainability is not an afterthought; it’s embedded in our clinical trial supply principles. We continuously seek ways to reduce our environmental impact through sustainable practices. This includes optimizing energy use, reducing waste, and considering the environmental impact of our supply chain decisions.
Clinical Trial Supply Planning:
Inventory Forecasting: Accurate inventory forecasting is crucial for clinical trial supply. It ensures the availability of necessary materials without surplus or deficit. This balancing act requires sophisticated modeling and a deep understanding of the clinical trial landscape to predict needs accurately.
Supply Chain Resilience: Building resilience into our clinical trial supply chain is about more than just contingency planning; it’s about creating a system that can withstand disruptions and maintain a steady flow of trial materials. This resilience is achieved through diversification of suppliers, robust logistics planning, and a proactive approach to risk management.
Analytical And Quality Assurance
Analytical Method Development and Validation: Analytical method development and validation are critical components of drug development and chemistry manufacturing controls (CMC). The goal is to ensure that the methods used to measure the identity, purity, potency, and stability of drugs are accurate, precise, and reliable. Analytical methods are indispensable tools for assuring the quality, safety, and efficacy of pharmaceutical products throughout the drug development process. The development of analytical methods involves a systematic approach to evaluating and selecting suitable methods that are sensitive, specific, robust, and capable of measuring the target attribute within acceptable limits of accuracy and precision. Method validation is the process of demonstrating that an analytical method is suitable for its intended use and capable of producing reliable and consistent results over time.
Quality Assurance in Clinical Trial Supply: Quality assurance encompasses a comprehensive quality management system that meticulously oversees every stage of production to ensure excellence. It includes rigorous in-process controls and thorough final product testing, which are the pillars of quality assurance in clinical trial supply. The integration of Quality by Design (QbD) principles into formulation development from the outset is a strategic approach in clinical trial supply operations, prioritizing quality and efficiency. Through risk assessments and Design of Experiments (DoE), critical quality attributes are identified and controlled, ensuring the highest standards of product integrity.
Quality by Design (QbD) in Formulation Development: QbD is a systematic and holistic approach that emphasizes the importance of understanding the impact of formulation and process variables on product quality and properties. It covers the entire product lifecycle, from development to commercialization, and focuses on the identification of the targeted product profile (TPP) and control of critical quality attributes (CQAs) that are important for product performance and safety.
Clinical Trial Supply Chain Optimization: Efficient logistics management is crucial in clinical trial supply, ensuring that products are delivered on time and in compliance with regulations. Inventory optimization strategies are implemented in the clinical trial supply chain to balance supply and demand effectively. Advanced mathematical analyses such as Monte Carlo simulations, as well as artificial intelligence techniques like machine learning, are employed to optimize the clinical trial supply.
Clinical Trial Supply Risk Mitigation: Comprehensive contingency planning is included in clinical trial supply services to address potential risks and ensure uninterrupted supply. Regulatory compliance monitoring is continuously conducted to anticipate and swiftly adapt to changes in regulatory requirements. Typical go-to mitigation strategies include updating the IRT configuration to minimize drug transfers to sites, slowing down or halting recruitment, and performing depot-to-depot shipments.
Pre-Formulation Analysis in Drug Development: Pre-formulation studies are an essential component of the drug development process, providing the scientific basis for formulation development. They give the physical, chemical, and mechanical properties of a new drug and help researchers choose what ingredients (excipients) should be used in the preparation.
Analytical And Quality Control in Clinical Trial Supply: In clinical research, the quality control process assures internal consistency by conducting periodic operational checks at every stage of the trial process and data handling to verify the compliance of the trial process and reliability of the data.
Regulatory Compliance Monitoring in Clinical Trials: Compliance in clinical trials is enforced through review and approvals by regulatory agencies and Institutional Review Boards (IRBs) to ensure that trial sponsors follow requirements related to the design of studies, participant recruitment, informed consent processes, data collection and management procedures, adverse event and safety reporting, record-keeping and reporting practices, and monitoring.
Supply Chain Standards in the Pharmaceutical Industry: The global medicine supply chain is a complex marketplace of manufacturers, suppliers, and distributors from many countries. Building a resilient supply chain requires predicting and preventing drug shortages, utilizing standards to foster quality, optimizing manufacturing capacity, and strengthening regulatory frameworks.
Global Distribution Network
Strategic Network and Seamless Logistics: The establishment of a strategic network of distribution centers is not just about expansive reach; it’s about intelligent placement. These centers are the linchpins of the supply chain, ensuring swift and reliable delivery to global markets. Seamless logistics, achieved through partnerships with leading international carriers, are crucial for navigating the complexities of cross-border transportation, which is vital for the inherently global nature of clinical trials.
Specialized Temperature-Controlled Shipping: For temperature-sensitive products, specialized shipping is paramount. Customized cold chain solutions, encompassing refrigerated and frozen options, are tailored to maintain product integrity. Advanced stability measures, including insulated packaging and temperature-controlled vehicles, are indispensable for preserving the products throughout their journey.
Cutting-Edge Packaging Technologies: Innovations in packaging technologies, such as smart packaging capable of monitoring environmental conditions, have revolutionized product maintenance during transit. The selection of damage-resistant materials ensures the supplies withstand the rigors of international shipping, providing an additional layer of protection.
Risk Management: Risk management in clinical trial supply involves proactive and reactive strategies. Proactive plans are developed months before a trial begins, using data to simulate and forecast trial needs, optimizing supply strategy, and minimizing drug waste. Reactive plans involve real-time monitoring and swift action to address any anomalies during transit, ensuring supply chain integrity.
Scientific Approach To Logistics: A scientific approach to logistics is characterized by protocols driven by scientific rigor, particularly for products requiring strict temperature controls. Stability testing under simulated transit conditions is standard practice, ensuring packaging solutions maintain product integrity. Collaboration with regulatory experts ensures compliance with pharmaceutical shipping regulations.
Clinical Trial Supply Chain Efficiency: Efficiency is achieved through optimized routing and scheduling, reducing transit times and costs. Effective capacity planning ensures the supply chain can handle varying volumes without compromising delivery timelines.
Sustainability: Sustainability in the supply chain is addressed through the use of eco-friendly packaging materials and green logistics practices, reflecting a commitment to minimizing environmental impact and reducing the carbon footprint of distribution activities.
Regulatory Expertise
In-Depth Regulatory Acumen: Our team’s profound knowledge spans across major regulatory bodies such as the FDA (U.S. Food and Drug Administration), EMA (European Medicines Agency), and PMDA (Pharmaceuticals and Medical Devices Agency of Japan). This expertise is not merely superficial; it involves an intimate understanding of the regulatory frameworks, guidelines, and approval processes unique to each body. This depth of knowledge ensures that we can adeptly navigate through diverse regulatory environments, which is crucial for the global clinical trial supply chain. It allows us to anticipate and mitigate risks, streamline approvals, and maintain a clear pathway through the complexities of global drug development and distribution.
Expansive International Expertise: Our capabilities extend beyond the borders of common regulatory territories. We are adept at maneuvering through the complexities of international regulatory landscapes, including the nuanced markets of emerging economies. This skibenefits the clinical trial supply process by ensuring that no matter where a trial is conducted, our understanding of the local regulations will facilitate a smooth operation. We have established relationships with local regulatory experts and have a track record of successful navigation through varied regulatory challenges, ensuring that our clients’ clinical trials can proceed without unnecessary delays or compliance issues.
Comprehensive Regulatory Submissions and Documentation:
Dossier Excellence: The preparation of a regulatory dossier is an art and a science, requiring meticulous attention to detail and comprehensive knowledge of the required information. We prepare extensive dossiers for regulatory submissions, ensuring each document is crafted with accuracy and completeness. This practice enhances the reliability of our clinical trial supply services and ensures that regulatory bodies receive all the information they need to make informed decisions.
Advanced eCTD Proficiency: In the era of digital submissions, our expertise with the Electronic Common Technical Document (eCTD) format is a significant advantage. This deep familiarity streamlines the submission process, supporting efficient clinical trial supply management. Our team is trained in the latest eCTD software and stays abreast of updates to submission portals, ensuring that our electronic submissions are not only compliant but also optimized for review by regulatory agencies.
Strategic Regulatory Strategy and Planning:
Lifecycle Regulatory Strategy: Strategic regulatory planning is not a one-time task but a continuous process embedded throughout the drug development lifecycle. From preclinical studies to post-marketing surveillance, our strategic planning ensures a smooth clinical trial supply operation. We work closely with our clients to develop a regulatory strategy that aligns with their product development goals, timelines, and market aspirations.
Pathways for Approval Expediency: In the competitive pharmaceutical industry, time is of the essence. We proactively identify regulatory pathways that can expedite the drug approval process, such as Fast Track, Breakthrough Therapy, Accelerated Approval, and Priority Review designations where applicable. This proactive approach ensures timely market entry and effective clinical trial supply distribution, providing our clients with a competitive edge.
Rigorous Regulatory Compliance Assurance:
Robust Compliance Programs: Our compliance programs are not just robust; they are comprehensive, meeting and often exceeding the stringent requirements of Good Clinical Practice (GCP), Good Manufacturing Practice (GMP), and Good Laboratory Practice (GLP). These are the pillars of clinical trial supply integrity, and our commitment to these standards is unwavering.
Dynamic SOP Evolution: Standard operating procedures (SOPs) are living documents that must evolve with the changing regulatory landscape. We regularly update our SOPs to align with the latest regulatory guidelines, ensuring that our operations remain at the forefront of compliance. This dynamic approach to SOP management is essential for maintaining the highest standards of clinical trial supply.
Adherence to ICH Guidelines: Our meticulous compliance with International Council for Harmonisation (ICH) guidelines for pharmaceutical development is a cornerstone of our operations. These guidelines are critical for ensuring that our formulations and clinical trial supplies are accepted globally, facilitating international clinical trial supply and reducing the risk of regulatory setbacks.
Excellence in Documentation: Documentation is the backbone of regulatory filings, and our commitment to documentation excellence is unparalleled. We maintain comprehensive and meticulous records to support regulatory filings, demonstrating our dedication to regulatory excellence and clinical trial supply accuracy.
Expert Regulatory Navigation:
Deep Expertise in Compliance: Navigating the complexities of customs and import/export regulations requires more than just knowledge; it requires expertise. Our team possesses deep expertise in this area, ensuring seamless clinical trial supply logistics. We understand the nuances of international shipping, customs clearance, and import/export regulations, and we leverage this understanding to ensure that clinical trial supplies reach their destinations without delay or complication.
Alignment with International Standards: We ensure strict compliance with international trade agreements and local regulatory requirements, which is vital for the uninterrupted flow of clinical trial supplies. Our operations are designed to be flexible and adaptable, allowing us to quickly adjust to changes in international standards and maintain compliance at all times.
Quality Assurance in Regulatory Affairs:
Rigorous Quality Checks: Quality checks are an integral part of our regulatory submission process. We conduct rigorous reviews of all regulatory submissions to prevent errors and omissions, ensuring the integrity of every application. This attention to quality is a key factor in the dependability of the clinical trial supply chain.
Ingrained Culture of Compliance: A culture of quality and compliance is deeply ingrained within our organization. This culture reflects our commitment to regulatory excellence and clinical trial supply standards. We foster an environment where compliance is everyone’s responsibility, and this collective commitment to quality ensures that our operations consistently meet the highest standards.
Scientist Involvement in Regulatory Processes:
Scientific Interpretation by Experts: Scientists at Hycon play a crucial role in interpreting complex scientific data for regulatory submissions. Their expertise contributes to the precision of clinical trial supply and ensures that regulatory submissions are scientifically sound and robust.
Involvement in Protocol Design: Our scientists are not just bystanders in the regulatory process; they are actively involved in the design and review of study protocols. This involvement ensures that our clinical trial supplies are designed to meet regulatory standards from the outset, which is fundamental for successful clinical trial execution.
Comprehensive Regulatory Support Services:
End-to-End Regulatory Support: We offer comprehensive regulatory support services that cover the entire spectrum of regulatory activities. From pre-submission advice to meeting facilitation and diligent follow-up with regulatory agencies, our support ensures a robust clinical trial supply framework.
Proactive Query Management: Our assistance extends beyond submissions to include the preparation of responses to regulatory queries and the management of regulatory inspections. This proactive approach to query management maintains the integrity of the clinical trial supply chain and demonstrates our commitment to regulatory partnership.
Advanced Clinical Trial Supply Chain Management:
Strategic Sourcing for Excellence: Strategic sourcing is a critical component of our clinical trial supply chain management. We implement strategic sourcing to secure high-quality materials and services, optimizing cost and ensuring supply continuity. Our sourcing strategies are designed to be resilient and adaptable, allowing us to respond to changes in supply and demand with agility.
Enhanced Supply Chain Visibility: Our advanced tracking systems provide end-to-end visibility of the clinical trial supply chain. This visibility enables proactive management and response to any issues that may arise, ensuring that clinical trial supplies are delivered on time and in compliance with regulatory requirements.
Innovation in Clinical Trial Supply Chain:
Integration of Technological Advancements: We continuously integrate technological advancements into our clinical trial supply chain. These advancements enhance efficiency and responsiveness, allowing us to stay ahead of the curve in a rapidly evolving industry.
Agile Supply Chain Modeling: Our agile supply chain modeling allows for rapid adaptation to changing clinical trial supply demands and regulatory landscapes. This agility is essential for maintaining a responsive and resilient supply chain that can meet the needs of our clients and their clinical trials.
Why Choose An Integrated Solution?
Analysis of Integrated Clinical Trial Supply Strategy:
The integrated clinical trial supply strategy employed by Hycon is a testament to the company’s commitment to excellence in the realm of pharmaceutical research and development. This strategy is not merely a procedural framework; it represents a paradigm shift in how clinical trial supplies are managed, emphasizing the importance of a harmonious partnership between Hycon and the sponsor project teams.
The essence of this strategy lies in its ability to transform a traditionally complex and segmented process into a streamlined and cohesive operation. By fostering a collaborative environment, Hycon and the sponsor teams can work in unison, ensuring that the supply chain is not just a series of isolated steps but a unified journey towards a common goal: the successful completion of clinical trials.
This integration goes beyond mere cooperation; it involves a shared vision where both parties are equally invested in the outcome. The result is a dynamic process where decision-making is informed by collective intelligence, communication channels are clear and open, and professional relationships are strengthened, paving the way for future collaborations.
Expanding on Clinical Trial Supply Efficiency:
The acceleration of clinical trial supply efficiency is a critical factor in the race to bring new medications to market. Hycon’s approach to achieving this is multifaceted, involving a meticulous orchestration of tasks that are executed concurrently, thereby compressing the timeline without compromising quality or safety.
This methodical acceleration is not about cutting corners; it’s about intelligent planning and execution. It’s about identifying and leveraging opportunities to perform tasks in parallel, thus reducing idle time and ensuring that every moment is utilized effectively. By doing so, Hycon ensures that the medication under trial reaches the clinic significantly sooner, which can be a decisive factor in the highly competitive pharmaceutical industry.
Moreover, this approach underscores the importance of agility in the clinical trial supply chain. In a landscape where time is of the essence, the ability to adapt and respond swiftly to changing circumstances can make the difference between success and failure.
Enhancing Seamless Clinical Trial Supply Management:
The concept of de-risking the clinical trial supply chain is central to Hycon’s philosophy. By adopting a seamless management strategy, the company aims to eliminate the vulnerabilities associated with transferring projects between multiple providers. This strategy is akin to constructing a bridge over the chasms of uncertainty that often plague the supply chain.
Continuity is the cornerstone of this approach. By ensuring a seamless transition between phases and providers, Hycon mitigates the risk of knowledge gaps that can arise during handovers. This continuity is not just about maintaining a steady flow of supplies; it’s about preserving the integrity of the data, the consistency of the methodology, and the momentum of the trial itself.
FAQs
Here are some frequently asked questions about Clinical Trial Supply
Clinical Trial Supply refers to the process of manufacturing, packaging, labeling, and distributing investigational medicinal products (IMPs) for use in clinical trials. It is crucial in ensuring that clinical trial materials are produced and distributed in a timely and compliant manner, enabling efficient and accurate testing of new drugs or therapies in clinical settings.
Our CDMO offers comprehensive services related to Clinical Trial Supply, including:
- Formulation development: Customized formulation of drug products suitable for clinical trials.
- Manufacturing: Scalable manufacturing of investigational medicinal products (IMPs) for all phases of clinical trials.
- Packaging and labeling: Customized packaging and labeling of clinical trial materials to meet regulatory requirements.
- Distribution: Global distribution of clinical trial materials to investigator sites or central depots.
- Supply chain management: End-to-end management of the clinical trial supply chain, including inventory management and forecasting.
- Regulatory support: Assistance with regulatory submissions and compliance with Good Manufacturing Practice (GMP) regulations.
We adhere to strict regulatory standards, including Good Manufacturing Practice (GMP) regulations, throughout the entire Clinical Trial Supply process. Our facilities are regularly inspected by regulatory authorities, and our quality control processes include rigorous testing of raw materials, in-process materials, and finished products. We also implement robust quality assurance protocols, including validation and stability studies, to ensure our products meet all regulatory standards.
Yes, we have specialized facilities and containment systems designed to safely handle controlled substances for clinical trials. Our team is experienced in managing the unique challenges associated with these substances, including stringent regulatory requirements and the need for specialized equipment and safety protocols.
Our production capacity is flexible and scalable to meet the needs of our clients, ranging from small-scale batch production for early-phase clinical trials to large-scale manufacturing for late-phase clinical trials. Our facilities are equipped with state-of-the-art machinery for granulation, compression, encapsulation, and coating, allowing us to efficiently produce a wide range of batch sizes with high precision and consistency.
We have extensive experience in managing cold chain logistics for clinical trial materials that require temperature-controlled storage and distribution. Our facilities are equipped with cold storage units and temperature monitoring systems to ensure the integrity of temperature-sensitive products. We work closely with trusted logistics partners to maintain the cold chain throughout the supply chain, from manufacturing to delivery to investigator sites.
While confidentiality agreements restrict the details we can share, we have successfully partnered with numerous pharmaceutical companies to supply clinical trial materials for a variety of therapeutic areas, including oncology, infectious diseases, and rare diseases. Our collaborative approach and commitment to quality have enabled us to support our clients' clinical trial programs effectively.
Our approach to forecasting and managing inventory for clinical trials is data-driven and collaborative. We work closely with our clients to understand their trial protocols and enrollment projections. Using historical data, we develop accurate forecasts for each clinical trial and proactively manage inventory levels to ensure continuous supply throughout the trial duration.
Starting a project with us is straightforward. Interested pharmaceutical companies can contact us through our website, email, or phone to schedule an initial consultation. During this consultation, we discuss the project scope, objectives, and timelines. Following this, we provide a proposal outlining our services, timelines, and cost estimates. Upon agreement, we initiate the project with a kick-off meeting to align on project details and establish communication protocols.
Our CDMO is committed to providing high-quality, compliant, and reliable clinical trial supply services. Our team provides adaptable on demand clinical manufacturing and supplies to provide clinical trial material deliveries at record time with quality in mind. Our team of experts is dedicated to delivering tailored solutions that meet the unique needs of each client, ensuring seamless collaboration and successful outcomes.