Pharmaceutical developers aim for cost-effective oral medications that work well. This can be challenging, requiring an understanding of client, patient, and provider needs. To succeed, developers must define the target profile, study the drug’s properties, conduct trials, solve solubility issues, ensure stability, and optimize delivery while minimizing costs and time.
Developing a Target Therapeutic Profile Creating the target therapeutic profile (TTP)
Developing a new drug is complex, requiring an understanding of many factors like efficacy, safety, and success. The Target Therapeutic Profile (TPP) is crucial and outlines the drug’s characteristics. To make a good TPP, consider factors like the condition it treats, patient details, dosage, safety, how it works, and cost.
Strategic planning at the start of drug development is crucial. It can improve results, make the process smoother, and reduce costs. Creating a clear and detailed Target Therapeutic Profile (TPP) makes decisions about doses and formulations easier. This helps with product development, partnerships, attracting investors, and getting regulatory approvals faster.
Furthermore, the creation of a TPP should be a collaborative effort that involves various stakeholders, including researchers, clinicians, regulatory agencies, and patients. The TPP should be continuously updated and refined as new data becomes available, and it should be leveraged as a decisive factor in the go/no-go decision-making process, ideally before the commencement of Phase I trials.
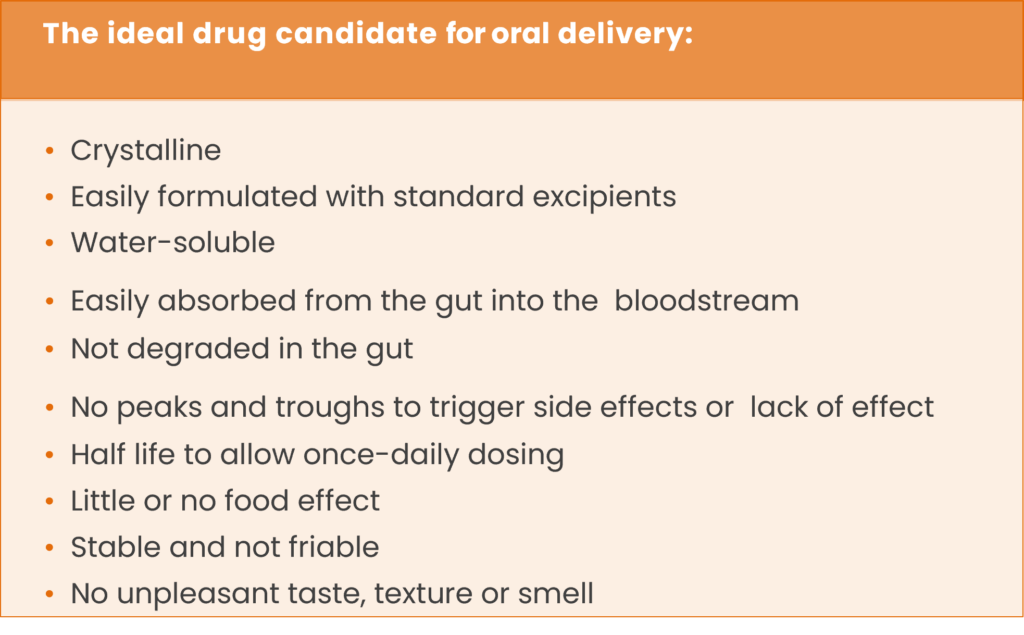
Investigating the Physiochemical Attributes of Molecules for Optimal Oral Formulation
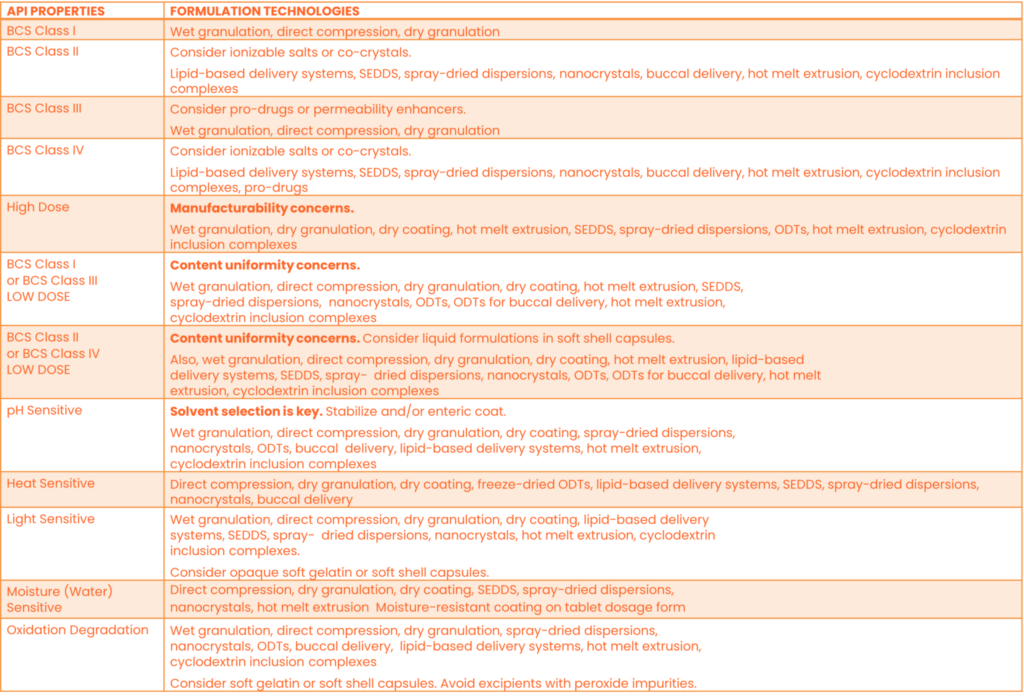
Understanding the characteristics of molecules is important when making oral medications. Two important factors are permeability and solubility. They affect how well the drug is absorbed and used by the body. The FDA has four categories for drugs based on these factors. Combining these with the target profile helps in making the right medication for preclinical and early clinical trials. Rene Pharma, a known pharmaceutical company, uses a special tool to suggest the best way to make oral medicines work better. This tool makes decisions easier and helps improve the results of the medicines.
Incorporating mathematical models can be instrumental in predicting the influence of a drug and its delivery system on drug release. To expedite the process, multiple simulations should be performed, followed by the identification of the most favorable simulation, conducting tests on it, and iteratively refining it to attain optimal results.
Attaining Preclinical and Clinical Proof of Concept (PoC)
Pharmaceutical and therapeutic development is a challenging and expensive, and it is essential to expedite the delivery of drugs through various studies and onto the market to achieve a rapid return on investment and an extended period of market exclusivity. While developing an oral medication may potentially delay the process, parallel execution of development steps is needed to maintain speed. This involves leveraging mathematical models to predict the effect of a particular drug and delivery system on drug release.
By conducting multiple simulations, identifying the most optimal one, testing it, and refining it, the overall drug development process can be accelerated. Furthermore, formulation procedures do not have to follow a linear path. Preclinical and clinical trials can be initiated even without a finished formulation by conducting bridging studies to demonstrate bioequivalence among tablets, liquids, or capsules. Nevertheless, it is important to remember that the FDA requires one year of stability data for a given formulation when conducting studies of the final formulation.
Significance of Solubility in Drug Development
Solubility is crucial in the development of oral drugs as it enables their absorption through the gastrointestinal (GI) tract. It determines the drug’s ability to dissolve in GI fluids and enter the bloodstream, affecting its bioavailability and therapeutic efficacy.
Assessing drug solubility is a fundamental step in early drug development, preferably during the preclinical phase. Identifying solubility issues early allows for timely intervention and formulation optimization. Delaying their detection can lead to significant difficulties and increased costs in later stages.
Significance of Permeability in Drug Absorption
Permeability is another vital factor influencing oral drug absorption. It refers to a drug’s ability to cross biological barriers, such as the gut wall, and enter the systemic circulation. Both solubility and permeability impact drug bioavailability, with solubility influencing dissolution in GI fluids and permeability determining the drug’s ability to traverse biological membranes.
The Biopharmaceutics Classification System (BCS) categorizes drugs based on solubility and permeability. This classification aids in understanding absorption challenges and guiding formulation strategies. BCS classifies drugs into four categories:
- High solubility and high permeability (Class I)
- Low solubility and high permeability (Class II)
- High solubility and low permeability (Class III)
- Low solubility and low permeability (Class IV)
Enhancing Solubility: Techniques and Innovations for Better Drug Absorption
For drugs with poor solubility, various techniques can enhance solubility and dissolution rate. These include particle size reduction through micronization or nanosizing, utilization of solubilizing agents or cosolvents, solid dispersion technologies, cyclodextrin complexation, pH adjustment, and lipid-based formulations. These approaches aim to increase the drug’s concentration in solution, improving absorption and bioavailability.
Methods such as changing particle size, using self-emulsifying systems for lipophilic drugs, and softgel technologies improve solubility. Hot melt extrusion blends drugs with polymers, applying heat to create a solid solution for different dosage forms. Renejix’s technology speeds up drug development safely and effectively.
To evaluate solubility and bioavailability, researchers measure solubility in simulated gastric fluid and assess the drug’s ability to penetrate the gut wall. Companies increasingly measure solubility early in development, starting from lead optimization, and set requirements to exclude molecules below a certain solubility level. Variations in solubility and bioavailability can impact drug safety and efficacy by altering patient exposure to the active component. Inadequate exposure may lead to no effect, while excessive exposure can result in increased side effects.
Ensuring Formulation Stability and Reliable Strength
Ensuring the stability and robustness of drug formulations is critical to maintaining consistent drug efficacy and patient safety. To achieve this, the final oral formulation must possess physical resilience that can withstand the rigorous demands of packaging, transportation, and storage. This requires the use of robust materials and formulation strategies that can withstand various stressors, including environmental factors such as temperature and humidity. Moreover, the formulation must be designed to ensure consistent drug potency and performance, regardless of whether it is consumed immediately after production or several months or years later.
To meet stability and strength standards, a minimum shelf life of 18 to 24 months is essential, with an ideal goal of up to five years. This extended shelf life is vital for products used in rare diseases or long-distance shipping, as pharmacies may store them for a long time. Ensuring stable drug formulations is crucial for patient safety and effectiveness, preventing degradation or contamination.
The manufacturing process must be dependable and rugged, with simplicity being key to achieving this. A reproducible manufacturing process is necessary to ensure that the final drug product meets the exact specifications required for its intended use. This involves using high-quality raw materials, employing appropriate manufacturing techniques, and subjecting the finished product to rigorous quality control testing.
Enhancing Drug Stability with Coatings
Coatings are one of the various techniques used to enhance drug stability and robustness. For instance, coatings can significantly improve the physical stability and robustness of oral capsules and tablets, particularly those that are delicate. Coatings applied to tablet or capsule formulations can also regulate drug release by providing a shield against degradation as the drug moves through the gastrointestinal tract. The selection of the appropriate coating material and formulation strategy is critical to achieving the desired level of stability and robustness.
Enhancing Delivery for the Targeted Therapeutic Profile
Optimizing the delivery technology and dose forms is a critical step in drug development to meet the specific requirements of the targeted therapeutic profile. The process involves choosing from a range of options such as potent solutions, robust syrups, effective elixirs, resilient suspensions, powders for reconstitution, highly dispersible/effervescent tablets, chewable tablets, rapidly disintegrating tablets, potent tablets, powerful sprinkles, oral powders, granules, and durable capsules.
The goal is to make a drug form that doesn’t change the drug’s properties. Sometimes, there are issues in making the drug early on, and we need to find a solution. Simplicity is often better for manufacturing and costs. Choosing the right form for patients is important, guided by the target profile. The condition matters; people like pills for pain but prefer liquids for coughs. For rare diseases, shelf life matters more than cost.
Conversely, for antihypertensive drugs with many competitors, the frequency of the dose and cost per dose are critical factors.
To sum up, optimizing the delivery technology and dose forms in drug development can lead to the development of an ideal dosage form that meets the target therapeutic profile’s requirements without changing the drug’s properties. Ultimately, this can ensure optimal patient care.
Targeted Patient Cohorts
Drug delivery must consider different patient needs. Young children may prefer liquids, while older kids may like chewable tablets, and adults may be fine with pills. Some older patients may have trouble swallowing pills. Special formulations can help, like liquids or fast-dispersing forms that mix with food or drinks. Devices like syringes, cups, and spoons can make dosing safe for both the elderly and children.
Furthermore, when it comes to adolescents, adults, and active elderly individuals, they are more likely to prefer capsules and tablets due to their practicality and inconspicuous nature. These solid dosage forms are often easier to handle, carry, and consume compared to other forms. They offer convenience, as they can be taken anywhere without the need for special storage conditions or preparation.
More Drug Delivery Options: Transdermal Patches and Inhalers
Transdermal patches provide a convenient method of drug delivery, especially for long-term treatment, as they can be applied to the skin and deliver the medication gradually over an extended period. Inhalers, on the other hand, are commonly used for respiratory conditions, providing a direct and efficient route of drug administration to the lungs.
Pediatric Medication Formulations and Dosage Adaptability
To account for the extensive range of ages and sizes, formulations for children must be adaptable, ranging from birth to 18 years old, to allow for dosage calibration based on age and weight. In addition, metabolic differences may require higher or lower doses. The difference in dosage between young babies and adolescents can be as much as 50-fold. Children under two years of age also have variations in gastric pH and gastrointestinal motility, which can affect the rate of delivery of controlled-release medications. Mini-tablets or capsules with a diameter of 1-2mm are an excellent option for children due to their ease of swallowing. However, liquid medications are practical for certain dose sizes, primarily for children, and tablets must be of the appropriate size for easy swallowing. Splitting the dosage allows for calibration. In a study of children aged six months to six years, 2mm uncoated tablets were found to be as well-accepted as sweetened syrups.
Enhancing Oral Medication Options for Children
Capsules containing pellets or mini-tablets provide a broader range of dose strengths and can be conveniently dispensed using a tablet dispenser, offering additional options for oral medication administration. It is important to note that crushing tablets is not recommended, and if a tablet needs to be divided, it should be split into two equal parts. When it comes to children’s medications, it is advisable to administer them no more than twice daily whenever possible. Considering taste, scent, and texture becomes crucial, particularly for oral medications intended for children. The use of gelatin capsules was introduced in 1834 to mask the taste of drugs, and contemporary methods include incorporating flavors, aromas, or sweeteners, coating tablets with polymers, liquids, or sugars, employing encapsulation, microencapsulation, granulation techniques, or utilizing taste suppressants and potentiators.
Enhancing Drug Dosage: Profile Analysis
To optimize drug delivery and minimize variations in safety and efficacy, various strategies can be used. One approach is using advanced drug delivery systems like nanoparticles and microparticles to precisely control drug release. Another technique is using different tablet formulations with unique coatings or cores to achieve various release rates or target specific body areas. Gastro-resistant coatings can protect drugs from the stomach’s acidity and ensure release in the intestine where absorption is better. These methods enhance drug safety and effectiveness and are important in developing new drug formulations.
Designing Patient-Centric Drug Formulations: The Significance of Color and Shape
Pharmaceutical manufacturers often prioritize the cheapest and most straightforward option: a plain white pill at a single dose. However, this strategy may prove inadequate for patients who consume multiple medications at varying intervals throughout the day. A profusion of small, white pills can lead to confusion, making it challenging for patients to track their medication. To address this issue, FDA regulations encourage manufacturers to produce drug formulations that facilitate the distinction of one medication from another by employing color, shape, or size.
Color and shape are pivotal components that can augment acceptability, brand recognition, and generate differentiation among various brands and generics. For instance, Nexium is distinguished by its purple hue, while Viagra sports a blue triangular shape. By incorporating images of unique shapes, colors, and designs into the FDA’s approval process, drug manufacturers can create distinctive and recognizable medications.
Implementing approaches such as color-coding of tablets can significantly mitigate medication errors, enhance compliance, and amplify recognition, especially among older patients with multiple medications and individuals with reduced dexterity who struggle to handle small pills. By prioritizing patient-centric formulations, drug manufacturers can bolster medication adherence and improve overall health outcomes.
Cost Considerations in Drug Manufacturing
When considering drug manufacturing costs, it’s essential to weigh the expenses carefully. While drugs with high-value ingredients and little competition have minimal cost impact during oral dose development, generic drugs need to control manufacturing costs to maintain profitability. This makes simple white pills an attractive choice. Additionally, a well-designed oral drug can enhance patient compliance and treatment outcomes, a crucial factor in health economics for both payers and patients. The cost of goods sold typically accounts for only 5% of the final drug price, so even if a pill costs one dollar to produce, the actual manufacturing cost is just five cents. Although advanced drug delivery systems might increase costs by up to 40%, this still leaves a substantial gross margin of 93%.
Developing an Enhanced Pharmaceutical Product
Developing an enhanced pharmaceutical product entails placing a high priority on scientific considerations and formulating an optimal therapeutic approach that is both practical and pragmatic. This approach ensures that the drug product is not only safe and cost-effective but also highly efficient in treating patients. Additionally, the product should have versatile applications, ease of use, and convenience, all of which contribute to improved patient compliance and overall treatment outcomes.